Osteoarthritis is the most common form of arthritis. Find out more about what causes it and how to relieve your pain.
What is osteoarthritis?
Osteoarthritis (OA) is the most common form of arthritis and it affects millions of people worldwide. How OA will affect you can vary. For some, it causes only mild symptoms (e.g. pain and stiffness) that come and go – but for others, it can cause constant and severe problems. Any of your joints can be affected but it occurs most often in knees and finger joints.
What causes osteoarthritis?
In healthy joints, cartilage covers the end of each bone. This firm, rubbery material helps the joint to move smoothly and acts as a cushion, or shock absorber, between the bones. In OA, this cartilage can become damaged and can wear away, which can lead to pain and stiffness in the joint.
This is why OA is sometimes called ‘wear and tear’ arthritis. However, this doesn’t mean that it only affects older people whose joints are simply wearing out. While it’s true that OA is more common over the age of 65, it can occur at any age and usually begins to affect you from around 45.

Did you know?
The cartilage that cushions your joints is called hyaline (glasslike) because thin sections of it are translucent, even transparent.*
OA doesn’t necessarily get progressively worse over time. If OA does begin to worsen, bones may break down and develop growths called spurs, and bits of bone and cartilage can chip off and float around in the joint. In the final stages of OA, as the cartilage in your joints wears away, the connected bones can begin to rub together, leading to joint damage and more pain. Eventually, moving the affected joint can become very uncomfortable and painful.
What are the symptoms?
Symptoms of OA vary, depending on the joints affected and how severely they are affected. Some of the most common symptoms of OA include:
- Joint tenderness, pain and stiffness
- Joint appearing larger and more ‘knobbly’ than usual
- Cracking or grating sensations when you move your joint
- Decreased function or limited ability to move your joint
- Weakness and muscle loss around the painful area
- Bone spurs, which can form as bones rub together
If you have OA in your knee joints, you may find that they ‘give way’ beneath you or it becomes difficult to straighten your legs. It is likely that both knees will be affected by OA unless it occurs as the result of a prior injury or condition that affected just one knee.
If you have OA in your hands, you can get bony growth spurs at the edge of the joints. This can make your finger joints stiff, sore, swollen, tender and red, so doing things like typing or playing the piano can be painful. OA usually affects the base of the thumb, the fingertips and the middle finger joints.
*Hyaline cartilage | anatomy | Britannica.com. 2016. hyaline cartilage | anatomy | Britannica.com. [ONLINE] Available at: http://www.britannica.com/science/hyaline-cartilage
Who is at risk?
There are several factors that make it more likely you will develop OA, including:
- Obesity – being overweight puts more pressure on the joints such as the knees, which can make cartilage wear out more quickly. This is why overweight women have nearly four times the risk of knee OA compared with non-obese women, while for overweight men the risk is five times greater. However, obesity may play a part in increasing your risk of any type of OA, even OA in the hands.
- Gender – women are more likely to develop OA than men, especially over the age of 50.
- Age – the risk of developing OA increases as you get older.
- Joint injuries – if you damage your joints in an accident or while playing sports, you are more at risk of developing OA in that joint, even if the damage happened years ago.
- Your job – if your work puts a lot of repetitive stress on a particular joint, for example if you have to use your hands all day typing or cutting hair, you are more likely to develop OA due to overuse of that joint.
- Your genes – some people inherit a tendency to develop OA.
- Bone deformities – if you are born with malformed joints or defective cartilage you are more likely to develop OA.
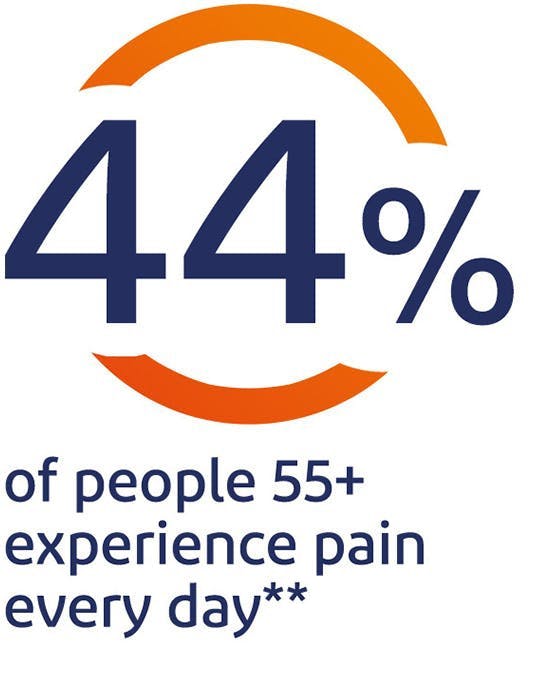
**GSK Global Pain Index Research 2014, report, p.8
Diagnosing and managing osteoarthritis
Your doctor can diagnose OA after examining the affected joint or joints. They may also recommend imaging, lab tests, or refer you to a specialist for further treatment.
Your doctor or pharmacist can advise you on medicines that can be used to help relieve the pain associated with OA. These include pain relievers such as paracetamol and non-steroidal anti-inflammatories (NSAIDs), which help to reduce pain and inflammation and are available over-the-counter as topical gels and creams, as well as tablets and capsules. In some cases, stronger prescription drugs may be required from a doctor.
Your pharmacist or doctor can offer advice on the best treatments to control your pain, as well as advise you on how to manage OA by losing weight, if necessary, and taking gentle exercise. As there is currently no cure for OA, these are important and form the main goals in the management of OA:
- Improve joint function
- Maintain a healthy body weight
- Control pain
- Achieve a healthy lifestyle
Learn more
What is inflammation?
Learn all about the processes that cause inflammation, why it happens and how it can make our bodies feel.
read moreHow to use Voltaren Gel to ease the pain of osteoarthritis
Osteoarthritis is one of the commonest causes of joint pain. Here we explain how Voltaren Gel can help to relieve the pain associated with osteoarthritis.
read moreAll you need to know about pain relief
Here we explain how different types of pain relief products work, to help you choose the best one for your pain.
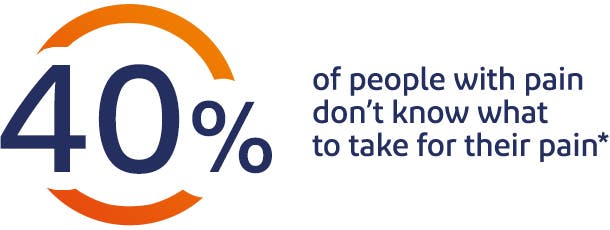
*GSK Global Pain Index Report 2014
Read More